Common causes of musculoskeletal dysfunction and painThroughout life the body is meant to move, stretch and exercise constantly. Sedentary life style and occupational faulty sustained posture (esp long hours at a computer), will lead to adaptive shortening of those muscles and ligaments held in a relaxed (shortened) and contracted position, whereas those muscles opposite become weakened, leading to muscular imbalance, causing chronic stress and strain with subsequent pain and disability. | Adrian De Vrij, Physiotherapist
|
 | Treatment for muscular imbalance consists of:
|
Classic Examples are:
1. Low back (lumbar) painBecause of shortened hip flexors (iliopsoas), which have their origin in the lumbar spine and pelvis insert into hip joints, cause low back strain and disability.
Tight hamstrings the iliotibial band (ITB) and eg piriformis (hip abductor), weak abdominals and overactive back extensors produce the same effect of muscular imbalance and subsequent low back pain. |  |
2. Neck (cervical) painMay follow sustained forward head posture, (A.K.A poking chin) with forward rolled (anterior) shoulders and slumped upper thoracic spine cause pain in these areas and in the upper three cervical vertebrae
(C1 to C3) become dysfunctional "cervico-genic headaches" may ensue (often called tension headaches) these headaches may affect any part of the head including "retro-orbital" pain (ie pain behind one or both eyes), and auditory disturbance (ringing, singing or buzzing in the ears,) disorientation, dizziness and diminished concern for others.
| Is your headache really a neck ache?For many people, feelings of pain and tension start at the top of the neck. As the pain worsens, it may spread to the back of the head, the temples, forehead or behind the eyes. Moving the neck or bending forward for a long time tends to make it worse. This happens because the nerves in the upper part of your neck are connected to the nerves in your head and face. So a disorder of the upper neck joints or muscles can cause referred pain to your head. Any of the following points suggest that your neck may be causing the headache:
|
3. Thoracic spinal painA sustained slumped posture will (eventually) cause thoracic spinal rigidity with a tendency to compress the (anterior), thoracic cage (chest). In addition to pain in the thoracic spine and the ribs, pain can sometimes radiate to the "sternum" and on occasion even into the throat (with mild nausea). This anterior chest pain may mimic cardiac disease and is known as "Pseudo-angina-pectoris". Of course actual cardiac pathology (incl stress related true angina pectoris) must be ruled out. It is possible for both Pseudo and True Angina Pectoris to be present simultaneously. Appropriate manual therapy for (non cardiac related) anterior chest pain, can usually produce immediate and dramatic relief (physical as well as psychological). |  |
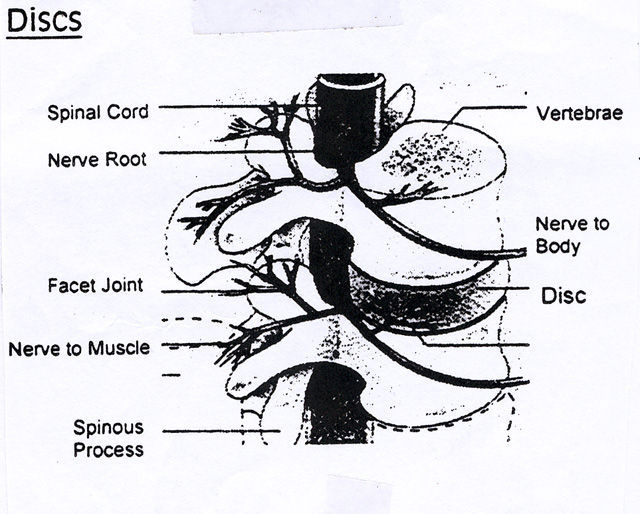
Herniated Discs
The vertebrae of your spine are separated by discs which have a fairly tough outer layer (the annulus fibrosis) with a soft interior (the nucleus pulposis) to cushion against the shocks and strains experienced as you move. These are subject to injury, disease, and degeneration with use over time. Certain activities, types of work and prolonged sitting posture increase the risk of being damaged and cause deterioration.
When the "Nucleus Pulposis" due to degeneration, pushes against the "Annulus Fibrosis" it may cause it to bulge or even rupture through a tear, a small fragment of the nucleus may become extruded and cause the emerging nerve root to be compressed with subsequent referred symptoms away from the site of compression. Herniated discs are also called protruding, bulging, ruptured, prolapsed or degenerated. There are fine distinctions between these terms, but all really refer to a disc that is no longer in its normal condition and / or position.
| A "slipped" disc is simply a popular name for one of the above terms. Most disc herniation takes place in the lower back (lumbar spine L4-S1). The second most common site of herniation is the neck (cervical spine). A herniated lumbar disc may send pain shooting through to your buttock and thigh into the back of your leg (sciatica), cervical disc herniation may cause symptoms in the shoulder, arm and hand - a herniated disc may also produce tingling and numbness and loss of muscular strength. Hemiated discs in the lumbar spine make it hard to get up when you've been sitting or lying down for sometime and cause pain when you move, even when you cough or sneeze. They sometimes produce pain elsewhere (referred pain). | 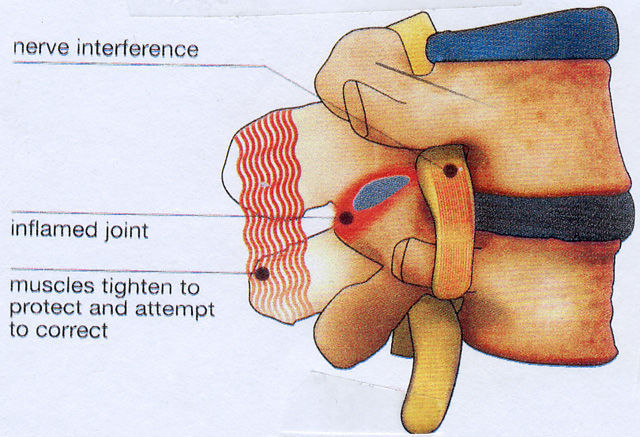 |
A spinal body prominence of say a large spinous process, may simply be a natural congenital variant in its shape and size known as tropism, whereas it may also be slightly out of alignment with the vertebrae above and below. A radiologist would normally describe these minor variations as being within normal limits, whereas many practitioners (other than physiotherapists) maintain, that the joint is "out" and should be manipulated back "in", the rewarding click (which is a natural cavitation occurrence) indicating that the joint has gone back "in" so then it is presumed that if the pain recurs, the joint has slipped "out" again and needs to be manipulated back "in".
| Any technique just on its own (eg 10-15 mins of manipulation only) cannot usually achieve a long term positive outcome and also carries the potential risk of flareup, (some call this the normal attempt and response of the body to correct itself as the spine is realigning itself which defies common sense). Incidentally it is within normal limits for the spinal vertebrae (spinous and transverse processes and vertebrae) to be somewhat out of alignment in anyone including all those without symptoms (particularly in the cervical spine, a spinal misalignment is only of any significance if it is not within normal anatomical limits as a radiologist would describe it). In any case in the cervical spine alone, there are some six anatomical barriers (impediments) that, prevent it to be realigned by manipulation, alone without the potential of causing damage. Multiple X-rays are generally unnecessary, so as to avoid excessive ionising radiation and subsequent health hazard, whereas MRI carries no such risk and it details the X ray does not. (they are also more expensive). |  |